Education and Research
Education Highlights
Through our teaching and scholarly efforts, we are showing how humanities-based palliative care education can help interprofessional teams provide artful and excellent care for all patients with serious illness.
The 3-Act Model
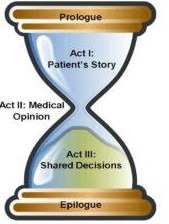
A goals of care conversation explores a seriously ill patient’s values, beliefs, and priorities in the context of the clinical situation, with the aim of providing care aligned with their values. With a nod to Aristotle, we designed a novel narrative approach to goals of care communication called the 3-Act Model (see hourglass figure). In recent studies, 3-Act Model training has led to learner proficiency in role-play as well as real-life clinical encounters, and has been the preferred method of trainees in the clinical setting:
Narrative Approach to Goals of Care Discussions: A Novel Curriculum (Wu, Kern, Dy, Wright) J Pain Symptom Manage
Narrative Approach to Goals of Care Discussions: Assessing the Use of the 3-Act Model in the Clinical Setting (Roberts, Wright, Dy, Wu) J Pain Symptom Manage
Integrating Narrative Goals of Care in the Medical Intensive Care Unit: Impact on Educational and Clinical Outcomes (Chatterjee, Roberts, Wu, Ahluwalia, Wright )
Narrative Approach to Goals of Care Discussions: Adapting the 3-Act Model Training to an Online Format (Roberts, Mehta, McWhirter, Dy, Wright, Wu) JPSM
Narrative interventions in the palliative care setting: a scoping review (Laskow, Small, Wu) J Pain Symptom Manage
2022 Outstanding Educational Program Award, JH Institute for Excellence in Education
Excellence in Education
“A simply outstanding educational program that was innovative, needs-based, iterative, and sustainable. The learner outcomes are measurable and impressive as was the scholarship that resulted from this educational curriculum.” – IEE
Groups of Learners We are Training
- Residents, Fellows, Physician Assistants, Physicians
- Nursing Students, Registered Nurses, Nurse Practitioners
- Pharmacy Residents and Students, Pharmacists
- Chaplain Residents
- Social Workers
- Interprofessional teams in key units and clinics
“I was blown away by the team at Bayview – it was amazing to witness the compassionate advocacy for patients and families and the seamless teamwork. I could tell the patients and families (and other staff!) really felt seen, heard, and valued through interacting with the PC team.”
Your ‘art of conversation’ and ‘the narrative 3 act approach’ were a God send to us. I believe to be under a doctor's care, who uses your techniques, will be a great blessing to everyone who is tied to that patient. Show those new doctors how to be great and the older doctors how to be greater in their practices.
Resident Palliative Interest Group (PIG)
Some of our greatest internal medicine residents are passionate about palliative care. With our guidance and support, they formed the Resident PIG, which has become a palliative hub within the residency.
PIG has broken bread together in homes and restaurants, hosted arts events, talked about fellowships and careers, and done educational outreach.
Research Notes
Bringing Stories to the ICU
 One of our current projects, funded by the Cambia Health Foundation Sojourns Scholar Leadership Award, is integrating the 3-Act Model (see above) in the Medical ICU at Hopkins Bayview. We are collaborating closely with leaders and team members in the ICU to integrate artful communication and systems change with the aim of improving person-centered care and systems outcomes.
One of our current projects, funded by the Cambia Health Foundation Sojourns Scholar Leadership Award, is integrating the 3-Act Model (see above) in the Medical ICU at Hopkins Bayview. We are collaborating closely with leaders and team members in the ICU to integrate artful communication and systems change with the aim of improving person-centered care and systems outcomes.
Palliative Interprofessional Collaborative for Action Research (PICAR)
The PICAR team consists of Danetta Sloan, PhD, David Wu, MD, Janiece Taylor, PhD, Natalie Regier, PhD, and Rebecca Wright, PhD,BSc (Hons), Ashley Booth, MSN, RN, Christy Swain, Program Administrator/Research Coordinator

We are grateful to partner with researchers at the Johns Hopkins School of Nursing and Bloomberg School of Public Health in doing important work at the intersection of palliative care and social justice. Together, we are aiming to better incorporate the voices of our patients and families and communities, in all their diversity, in the care of those with serious illness using participatory / collaborative / co-design approaches. Our conceptual framework is described in this publication, “A Call to Action to Address Disparities in Palliative Care Access: A Conceptual Framework for Individualizing Care Needs.”
One project we are working on, funded by the Hillman Foundation, is entitled: “A nurse-led approach to improving palliative care in the ICU for Black populations.” Rebecca Wright, PhD, BSc (Hons), is the principal investigator for the project, and co-investigators include Danetta Sloan, PhD, and David Wu, MD.
Another project, funded by the Johns Hopkins Institute for Excellence in Education, is “Partnering with community members to design culturally sensitive goals of care communication training.” David Wu is the principal investigator, and co-investigators include Drs. Wright and Sloan, Drs. Chapla and Orozco from our Division, and several incredibly talented Medicine residents, Drs. Ekene Ojukwu, Amarpreet Ahluwalia, and Kamini Kuchinad.
Neuropalliative Care 
Dr. Mehta leads multidisciplinary collaborations at both Johns Hopkins Bayview and Johns Hopkins Hospital with our colleagues in the Neurological, Neurosurgical, and Neurocritical Care departments to increase access to neuropalliative care.
Persons living with neurological illnesses have unique palliative care needs. Compared to other diseases, neurologic illnesses can result in significant limitations in people’s ability to think, communicate, and may cause memory deficits and personality changes. Communication skills for advance care planning and complex symptom management are critical palliative care skills that all neurologists should be comfortable with. The burgeoning field of neuropalliative care has developed to encompass these specific needs.
To increase access to neuropalliative care at Johns Hopkins, we have developed clinical, research, and educational partnerships with our neurology, neurosurgery, and neurocritical care colleagues. In the inpatient setting, our interdisciplinary team collaborates to provide support during family meetings for the NeuroICU and General Neurology wards. Our neuropalliative physician is embedded in the multidisciplinary Johns Hopkins Center for ALS Specialty Care, which is associated with the ALS Association.
A Sample of Our Team’s Publications
Defining Clinical Excellence for Palliative Care Specialists: A Concept Whose Time Has Come. (Wu, Mehta, Brewer, Sloan, Dy, McPherson, Dahlin) Am J Hosp Palliat Med. 2022.
Clinical excellence in palliative care. (Wu, Wright) Am J Hosp Palliat Med.
Models of outpatient neuropalliative care for patients with amyotrophic lateral sclerosis. (Phillips, Besbris, Foster, Kramer, Maiser, Mehta) Neurology. 2020.
Top Ten Tips Palliative Care Clinicians Should Know About Seizures at the End of Life. (Sharma, Besbris, Kramer, Daly, Singhal, Jones, Mehta) J Palliat Med. 2021.
Palliative Care Consults in an Inpatient Setting for Patients With Amyotrophic Lateral Sclerosis. (Mehta, Jackson, Wiedau-Pazos) Am J Hosp Palliat Care. 2021.
Primary palliative care education for trainees in US medical residencies and fellowships: a scoping review. [published online July 8, 2020]. (Paulsen, Wu, Mehta) J Palliat Med.
Covid-19-pandemic-response-development-of-outpatient-palliative-care toolkit based on narrative communication. (Roberts, Wright, Christmas, Robertson, Wu) Am J Hosp Palliat Med. 2020.
Hopes and Future Directions
Building on our success to date, in 5 years we aim to:
- have artful palliative care thoughtfully integrated throughout the hospital AND the community;
- have a robust interprofessional research program pursuing health equity in palliative care;
- keep growing, thriving, and bringing peace.